Your own virtual heart for non-invasive heart diagnostics
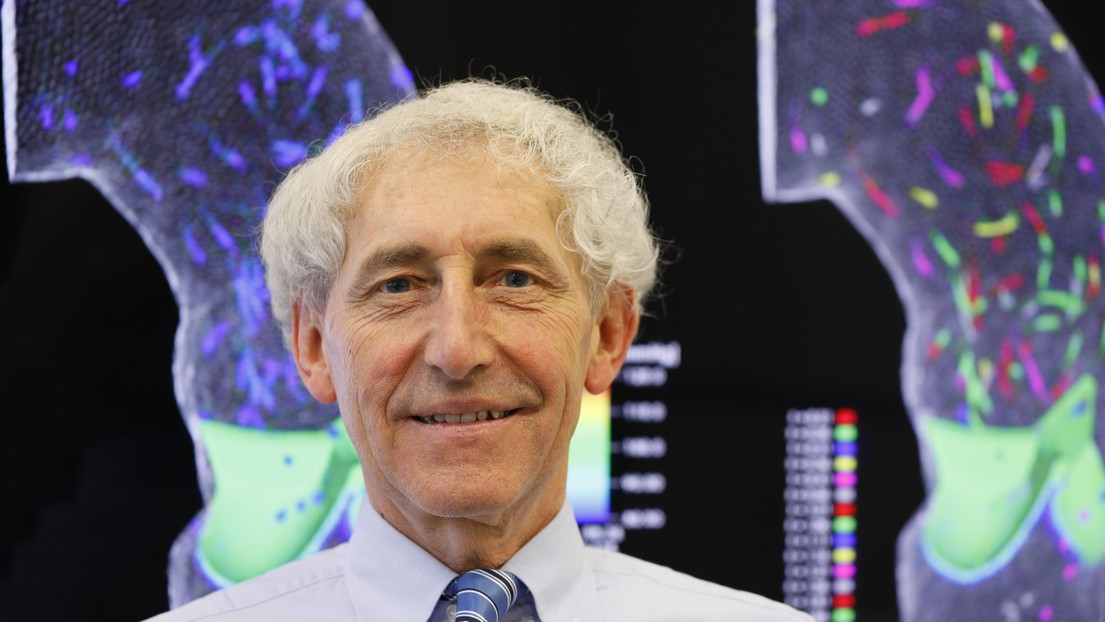
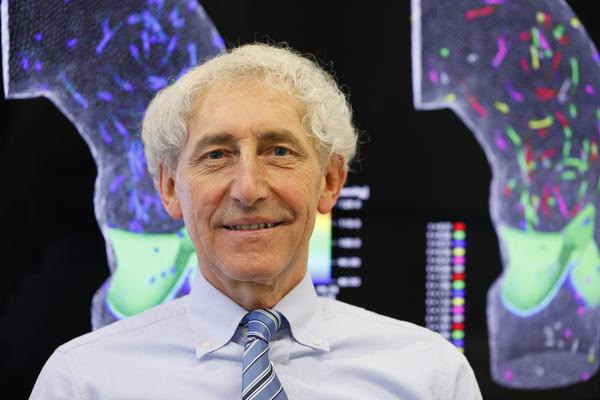
© 2017 EPFL / Hillary Sanctuary
EPFL mathematician Alfio Quarteroni and his team are building a virtual heart model based on personalized medical images that may one day help cardiologists and cardiac surgeons non-invasively diagnose pathological heart conditions. The team recently modeled and simulated the behavior of a patient’s aortic valve.
One day, a virtual version of your own heart pumping may help doctors diagnose heart disease and determine the best treatment for you, without the need of surgical intervention or other invasive clinical practices. EPFL mathematician Alfio Quarteroni’s goal is precisely this as he builds mathematical tools to simulate heart function with increasing accuracy and that can be personalized to your heart based on medical scans. He recently added the behavior of a patient-specific aortic valve to his overall functioning heart model. The results are published June 7th in Biomechanics and Modeling in Mechanobiology.
A personalized virtual heart for preventing cardiovascular disease
The human heart is an extraordinarily complex organ that pumps an estimated 180 million liters of blood, which would fill more than seven Olympic-sized swimming pools in one’s lifetime, thereby ensuring that oxygenated blood reaches the entire body. Cardiovascular problems may lead to malfunction, disease, or death. Heart disease causes 40% of deaths in the EU and costs an estimated 196 billion a year, yet 80% of acquired heart diseases and stroke episodes are preventable.
Quarteroni aims to help prevent or treat cardiovascular disease by providing a personalized virtual heart to patients, essentially a detailed mathematical description of a patient’s heart and how it functions – or malfunctions.
Every person’s heart is unique. Correctly modeling the intricacies of each individual heart therefore requires a customizable mathematical description of both its geometry and its dynamics. But doing so in a mathematically sound way is no easy task; it requires large amounts of patient-specific data and computational power to solve complex equations. Thanks to increasingly powerful computers, building a realistic virtual heart is becoming a reality.
How to build a virtual aortic valve
In constructing a virtual heart that is complete and functional, the aortic valve cannot be neglected. Quarteroni and his team recently added to their heart model the way blood flows from inside the heart into the aorta, taking into account the complex shapes and properties of the aorta’s physiological membranes: the valve leaflets.
“A mathematical description of the aortic valve and its interaction with blood flow exists in the literature, but not at this level of detail for a specific patient,” says Quarteroni.
From MRI scans of a patient, they reconstructed the shape of the aorta, which they represented using a 3D computational mesh. Using mathematical tools to characterize the mechanics of the valve, they described the movement of three triangular-shaped leaflets that make up the aortic valve. To determine how blood flows inside of the atria, the heart’s cavities, they next approximated and numerically solved the mathematical equations (Navier-Stokes) that describe viscous fluid dynamics, adapting them for a patient-specific geometry. Even with this preliminary work, it is a relatively easy task to personalize the model to another patient by using a new set of MRI scans.
As the director of iHeart, an EU-funded project, Quarteroni’s long-term vision is to build patient-specific virtual models of the entire cardiovascular system, including the heart, all of the body’s blood vessels, and of the approximately five liters of blood flowing through the body.
“If successful, iHeart will help clinicians to tackle important questions efficiently, both in diagnostics and treatment, with a tremendous impact for society,” says Quarteroni. “It will provide a unique, unprecedented research environment for exploring the heart with an immensely powerful and non–invasive mathematical microscope, making it possible to simulate cardiovascular disease, like carotid stenosis and aneuryisms that can affect the heart, the abdomen, the brain and other parts the body.”
Quarteroni believes that a personalized virtual heart model may become clinically available in less than a decade. Earlier prototypes of the virtual model may be developed and tested sooner, possibly within a five-year horizon. This will require significant investment in the development of robust mathematical and numerical tools to simulate heart function that is tailored to a specific patient.