Understanding the propagation of Alzheimer's Disease

© photos.com
The connections between neurons might play a role in neurodegenerative diseases, including Alzheimer’s Disease (AD). In a pioneering approach to studying how neurodegenerative diseases like AD spread within the brain, researchers at EPFL have developed a novel in vitro experimental method that allows them to connect healthy neurons with “infected” neurons and then observe the results.
How do neurodegenerative diseases like AD spread within the brain? Do the connections between neurons play a role in how these diseases develop, or is it simply that weaker nerve cells are affected first and stronger ones later in the course of the illness? These key questions, which have not yet been the object of much scientific study, are at the heart of a novel experimental method developed by Robert Meissner and Anja Kunze. The two EPFL scientists have designed a cell culture device with two compartments in which it is possible to “connect” healthy neurons and “sick” neurons via a neurite network. Their work will make it possible to conduct in-depht studies of how neurodegenerative diseases spread via the connections between neurons.
“Most work on AD focuses on biochemical mechanisms within the cells,” says Microsystems Laboratory 4 (LMSI4) Director Philippe Renaud, in whose lab the work took place. “In fact, AD starts in a specific area of the brain, the limbic system, and then spreads to other areas. This would tend to indicate that neural networks probably play a role in disease propagation.” The method and results were published in the journal Biotechnology and Bioengineering, and might well be applicable to the study of the propagation mechanisms of other neurodegenerative diseases, such as Parkinson’s Disease and Creutzfeld-Jakob’s (i.e., the human form of “Mad Cow”) Disease.
Connecting two separate neuron cell cultures
The team “connected” the two groups of cultured neurons in a custom-designed microfluidic-based cell culture device. The device has three compartments (see illustration). Microchannels measuring 50 to 100 microns were used to guide neurite outgrowths that linked thousands of neurons in the device’s two lateral compartments. In this way the healthy and “sick” neural cell populations were at once separate and interconnected, a situation that the research team refers to as a “co-pathological” state.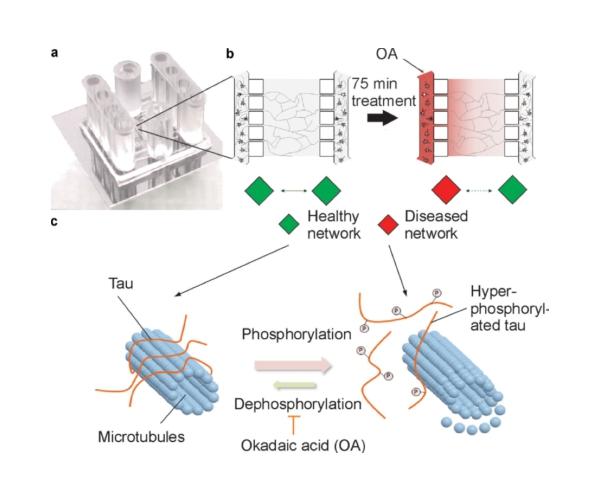
Making the neurons “sick”
To “infect” one of the two interconnected cell cultures, one of the compartments was exposed to Okadaic Acid (OA). OA makes neurons exhibit one main characteristics of AD by causing hyperphosphorylation of the Tau proteins in the cells. This is a hallmark of AD, and it leads to the progressive destruction of the neural networks as well as the neurons themselves. “We exposed the neurons to high doses of OA, and it killed them within 24 to 48 hours,” says Anja Kunze, co-author of the article detailing the new method. “But we could also try lower exposure levels and observe the results over longer periods of time. Our results thus far show that the healthy cells were contaminated after 24 hours. But more observations are needed before drawing any conclusions.”
An innovation that opens the door for further research
The new method has already aroused the interest of neuroscientists. “What’s really interesting is that they can precisely target the specific neural cell population they want to make sick,” says Patrick Fraering, an AD neuroscience specialist. “This method can be used for many types of tests, including tests for other neurodegenerative diseases. For instance, Parkinson’s Disease symptoms could be triggered in one of the compartments. Or you could try applying various candidate drugs as treatments on diseased cells.” All of this will sharpen our understanding of how these illnesses spread and increase the chances that it may one day be possible to contain the damage that neurodegenerative diseases do to the brain.