Targeting Astrocytes May Slow Alzheimer's Disease
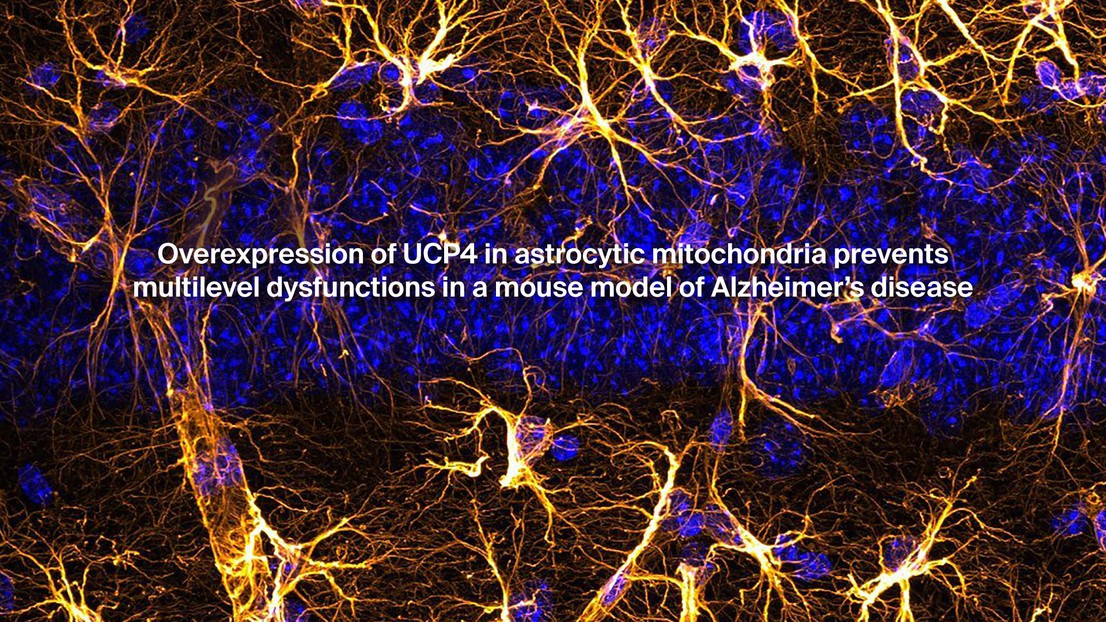
© 2023 EPFL
A new study published in the journal GLIA has found that targeting astrocytes, which are cells that play crucial functions within neuronal circuits, may be an effective strategy in preventing the decline of neurons in Alzheimer's disease (AD). The study, conducted by teams of researchers from the University of Lausanne and EPFL’s Blue Brain Project, found that overexpressing a specific protein in the astrocytes prevented many of the neurological changes seen in AD mice model and helped in preserving short term memory.
Alzheimer's disease is the most prevalent cause of dementia in elderly people and is characterized by progressive deterioration of memory, language, and cognition. The number of cases is increasing worldwide and at this time, none of the medications available can slow down or stop the disease progression. Current attempts to treat AD focus on countering neurotransmitter disturbances or target misfolded proteins. In a radically different approach, this study looked at targeting astrocytes to better support neuronal function. Astrocytes play crucial functions within neuronal circuits by providing metabolic and functional support, regulating biochemical composition in the space between neurons, and modulating synaptic transmission between them. Now, growing evidence points to an essential role of astrocytes in neurodegenerative diseases like AD. Early-stage AD is associated with hypometabolism and oxidative stress.
Working with the mice equivalent of AD, the researchers overexpressed a naturally present protein within the astrocyte mitochondria, their power plants. In promising results, the study found it prevented alterations of metabolite levels, hippocampal atrophy, reduction of the arborization of certain neurons, and preserved episodic-like memory in AD mice models.
"The findings suggest that targeting astrocytes and their mitochondria is an effective strategy to prevent the decline of neurons facing AD-related stress at the early stages of the disease," says Blue Brain scientist Maria Reva, who led the neuromodeling part of the study. "This underlines the links between the reduction of neuronal architecture and the alteration of signal propagation in the neuron, and how these in turn affect memory formation in the brain and cause hippocampal atrophy of neurons in AD mouse models” adds lead author and postdoctoral fellow Nadia Rosenberg.
The study adds to growing evidence that points to an essential role of astrocytes in neurodegenerative diseases like AD. "This research opens up a new avenue for treatment development and could potentially lead to therapies that slow down or stop the progression of the disease" adds Professor Jean-Yves Chatton, lead scientist at the University of Lausanne. ”We are thrilled that our simulation neuroscience tools could support this study, and look forward to many more such applications." concludes Professor Henry Markram, Blue Brain Founder and Director.
-----------------------
Authors and Affiliations
Department of Fundamental Neurosciences, University of Lausanne, Lausanne, Switzerland - Nadia Rosenberg, Francesca Binda, Leonardo Restivo, Pauline Depierre, Julien Puyal, Marc Briquet, Anne-Bérengère Rocher & Jean-Yves Chatton
Blue Brain Project, Ecole polytechnique fédérale de Lausanne (EPFL), Geneva, Switzerland - Maria Reva & Henry Markram
Neonomia, Geneva, Switzerland - Yann Bernardinelli
Cellular Imaging Facility, University of Lausanne, Lausanne, Switzerland - Jean-Yves Chatton
This work was supported by the Synapsis Foundation Alzheimer Research Switzerland, the Fondation Juchum, the Chafee Stiftung, and by the Blue Brain Project, a research center of the École polytechnique fédérale de Lausanne, EPFL, from the Swiss government’s ETH Board of the Swiss Federal Institutes of Technology.
Rosenberg, N., Reva, M., Binda, F.,Restivo, L., Depierre, P., Puyal, J., Briquet, M., Bernardinelli, Y.,Rocher, A.-B., Markram, H., & Chatton, J.-Y. (2022). Overexpression of UCP4 in astrocytic mitochondria prevents multilevel dysfunctions in a mouse model of Alzheimer's disease. GLIA, 1–17. https://doi.org/10.1002/glia.24317