Targeting “anti-tumor” genes to provide better treatment for leukemia
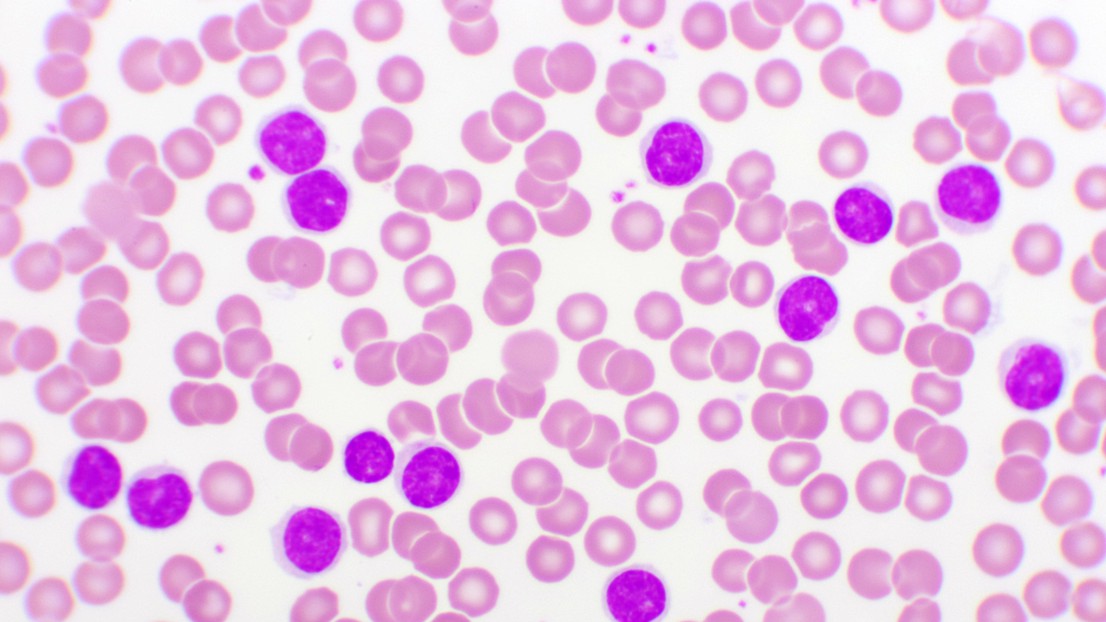
Blood smear of chronic lymphocytic leukemia (CLL), analyze by microscope. EPFL/ iStock
EPFL scientists discuss the possibility of offering personalized treatment for chronic lymphocytic leukemia by regulating the expression of a gene known for its “anti-tumorous” properties.
Chronic lymphocytic leukemia (CLL) is one of the most common blood cancers in adults. The disease originates in B cells – the part of the immune system that produces antibodies – and then evolves slowly, typically affecting older people. Today, the best method of treating severe forms of CLL is chemotherapy, potentially supplemented by healthy stem-cell transplants. But new therapies, possibly less invasive and more effective, are currently being developed, and they could be enhanced considerably by a deeper understanding of how genetics contributes to disease susceptibility.
An anti-tumor gene
Each individual has their genetic material stored in DNA within the nuclei of their cells. Variations in a single base in a given nucleotide sequence of DNA results in genetic differences between people. This is called nucleotide polymorphism, and can lead to differences such as a greater susceptibility to diseases like CLL. At EPFL’s Laboratory of Systems Biology and Genetics, headed by Prof. Bart Deplancke in the School of Life Sciences, scientists are attempting to unravel the mechanisms behind the formation of variable chromatin modules (VCMs), which are differentiated units in the genome that represents coordinated molecular behavior, leading to the expression or regulating the expression of a gene.
In certain cases, the variant seems to significantly slow the disease progression in patients
The scientists wanted to find a particular case of VCM which would allow them to target CLL. “We examined numerous VCMs for specific activities, and settled on one that we found particularly interesting because it seemed to control a gene that we understand fairly well, AXIN2. This gene is reputed to have ‘anti-tumorous’ properties,” says Deplancke. By concentrating on the VCM that regulates the expression of AXIN2 in B cells, the team discovered a variant that not only impacts at the molecular level, but also affects the phenotype in CLL patients. “This variant seems to mitigate the disease in two ways: it reduces susceptibility to leukemia; and in certain cases, it significantly slows the disease progression in patients,” says Deplancke.
The research was conducted in collaboration with Prof. Freddy Radtke’s laboratory at EPFL and the research groups led by professors Alistair Boettiger (University of Stanford), Gianluca Gaidano (Oncology Institute of Southern Switzerland), David Rossi (University of Eastern Piedmont), Christoph Plass (European Molecular Biology Laboratory), and Dr. Sebastian Waszak (Centre for Molecular Medicine Norway). The results were published in Nature Communications on 19 April 2022.
V/ happy with our lab's new OA paper: "A leukemia-protective germline variant mediates chromatin module formation via transcription factor nucleation" https://t.co/rLB1eP4n9f. Big tx to Gerard & collabs: @ABoettiger, @Toniai12, @sebastianw, @isrec_radtke et al. Feedback welcome! pic.twitter.com/kR5wHnzjjb
— Bart Deplancke (@BartDeplancke) April 19, 2022
New treatment possibilities
The researchers believe that regulating the expression of AXIN2, and therefor its “anti-tumorous” protein in B cells, could let CLL patients with this genetic variant live longer and better. To test these findings, the study’s lead author, Gerard Llimos, overexpressed the AXIN2 gene in mice severely affected by chronic lymphocytic leukemia.
“We noted that the tumorous cells where AXIN2 had been overexpressed proliferated much more slowly than those which did not express AXIN2,” says Deplancke. “This long-term disease is still difficult to mimic, but our study revealed two things. First, it may be interesting to know if a patient with CLL possesses this AXIN2 VCM in their DNA because that will provide information on their body’s capacity to fight effectively against the disease. Second, it opens the door to possible new therapies that involve augmenting a patient’s level of AXIN2 in a targeted way in order to slow disease proliferation, as Gerard was able to do in mice.”
Some drugs which can specifically target the AXIN2 variant have already reached clinical trials. Thanks to this research, personalized cancer treatments may soon be on the horizon.
This work was supported by a Swiss Cancer Research foundation grant (KFS-4275-08-2017), a Swiss National Science Foundation grant (310030_197082), and generous internal support by the EPFL. S.M.W. receives support from The Research Council of Norway (187615), the South-Eastern Norway Regional Health Authority, and the University of Oslo. P.L. and C.P. are supported by the German Cancer Aid project CO-CLL (#70113869). G.G. is supported by AIRC 5 ×1000 No. 21198, Associazione Italiana per la Ricerca sul Cancro Foundation, Milan, Italy.
A leukemia-protective germline variant mediates chromatin module formation via transcription factor nucleation. Gerard Llimos, Vincent Gardeux, Ute Koch, Judith F. Kribelbauer, Antonina Hafner, Daniel Alpern, Joern Pezoldt, Maria Litovchenko, Julie Russeil, Riccardo Dainese, Riccardo Moia, Abdurraouf Mokhtar Mahmoud, Davide Rossi, Gianluca Gaidano, Christoph Plass, Pavlo Lutsik, Clarissa Gerhauser, Sebastian M. Waszak, Alistair Boettiger, Freddy Radtke & Bart Deplancke, Nature Communications, 19 April 2022.