Smart Nanoparticles keep immunotherapy focused on cancer
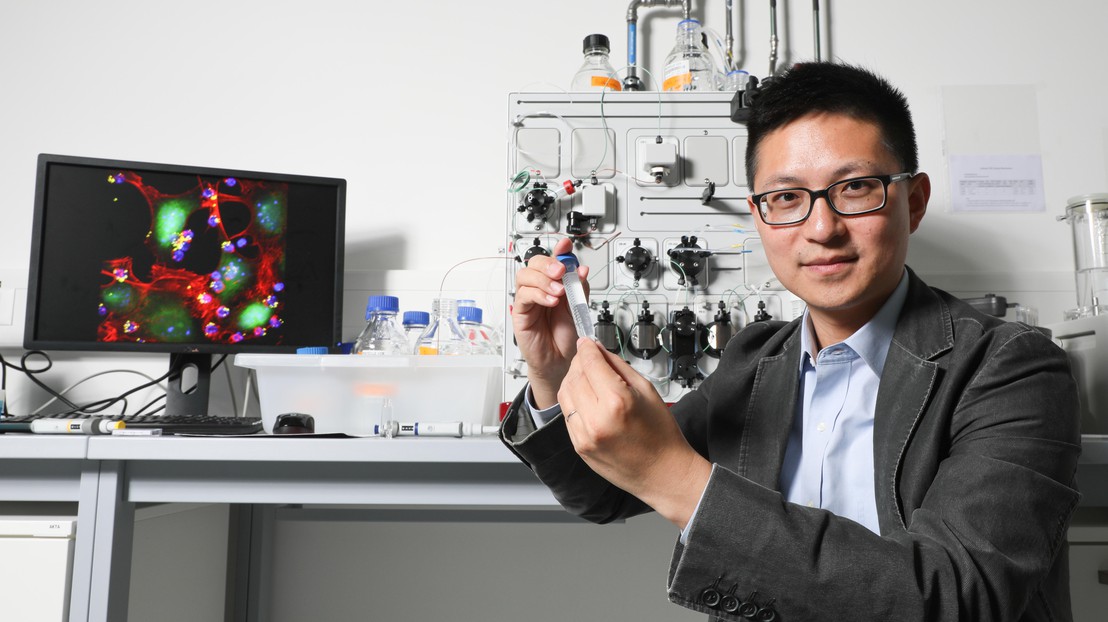
Professeur Li Tang© Alain Herzog / 2018 EPFL
MIT and EPFL researchers have developed a highly targeted and non-toxic method for battling cancer through immunotherapy. Their nanoparticle gel acts only on immune cells surrounding the tumor, without affecting the rest of the body.
Immunotherapy is a highly promising and innovative approach to battling cancer that works by enlisting the body’s natural defenses to attack cancer cells. By stimulating T lymphocytes, which play a key role in the human immune system, cancer researchers have already achieved unparalleled results in treating cases of leukemia and certain types of melanoma – a common form of skin cancer.
However, these treatments often raise problems of toxicity for the rest of the body and can have serious side effects.
The MIT and EPFL researchers addressed this challenge by developing a nanoparticle gel that can be used to control exactly where and when drugs designed to boost the immune cells are applied. Their method is more effective at stimulating the body's defenses and ensures that the drug acts only on the cancer tissue, without harming the rest of the body. This study, part of which was carried out at MIT, and another part at EPFL’s School of Engineering, has been published in Nature Biotechnology. It will be featured on the cover of the journal. Two patents covering the inventions have been licensed, and their method will soon be tested on patients by Torque, a firm based in Cambridge, Massachusetts.
Arming the cells that defend the body
Our immune system includes T cells, also called T lymphocytes, which are very effective at battling infections and viruses. But when it comes to cancer, although they recognize the enemy, they are powerless against it. The tumor disables them and prevents them from replicating, which results in their destruction. That's where immunotherapy comes in: this approach aims to safeguard the T cells’ defensive properties.
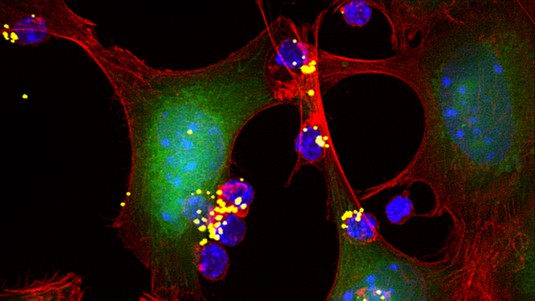
One form of immunotherapy consists of taking T-cell samples from a patient, modifying them and reinjecting them into the body. The resulting army of T cells can then destroy the cancer. The EPFL and MIT researchers opted for this approach, creating a “backpack” for the T cells that only opens when it comes into contact with a tumor. The backpack contains cytokine molecules that have been chemically bonded together by reticulation to form a nanogel. The backpack is attached to the T cell using CD45 antibodies and does not open until the T cells give off the right signals.
The T cells detect tumors thanks to the tumor antigens located on the surface of cancer cells. The T cells then activate their membrane receptors (T-cell receptors, or TCRs), which cause a chemical reaction – reduction-oxidation reaction, or redox – that modifies their immediate surroundings. An exchange of electrons causes the backpack to open and deliver high doses of cytokine substances to the T cells. The cytokine restores the T cells’ functioning, allowing them to proliferate again as normal and destroy the cancer.
No encapsulation, and unparalleled efficiency for drug transport
This technique offers a number of important advantages. For starters, no intermediary is required to transport the drug, as the backpack itself is made of cytokine substances. This technique can therefore deliver a much more complete treatment than conventional methods can. “Each particle contains almost 100% of the active substance versus only 10% achieved through encapsulation – where there is also the risk that the transporter will interfere with the drug,” says Li Tang, head of EPFL’s Laboratory of Biomaterials for Immunoengineering (LBI) and lead author of the study. Second, the controlled release of cytokine is a breakthrough. “The drug will be delivered only to the sick cells, and nothing will happen to the healthy tissues. There, the cytokine in the T-cell backpack will not be released or cause side effects in healthy tissues.
Two types of T-cell-based immunotherapy have been on the market since 2017 and have proven to be highly effective for treating leukemia and lymphoma. The EPFL and MIT researchers’ method could improve these treatments and be used on different types of cancer, in particular, solid tumors.
-----
The research project began at MIT and was completed at EPFL, in the Laboratory of Biomaterials for Immunoengineering (LBI), headed by Li Tang in the School of Engineering (STI).

This work was supported in part by the Ragon Institute of MGH, MIT, and Harvard, the Melanoma Research Alliance (award 306833), the NIH (Koch Institute Support (core) grant P30-CA14051 from the National Cancer Institute and CA172164), and the Koch Institute Marble Center for Cancer Nanomedicine. L.T. was funded by a Cancer Research Institute (CRI) Irvington Postdoctoral Fellowship, and Y.Z. was supported by a National Science fellowship from the Agency for Science, Technology and Research, Singapore. L.T. and Y.-Q.X. were supported by the ISREC Foundation, with a donation from the Biltema Foundation, and the Swiss National Science Foundation (project grant 315230_173243). M.V.M. was supported by NIH CA K08166039. D.J.I. is an investigator of the Howard Hughes Medical Institute.
Li Tang, Yiran Zheng, Mariane Bandeira Melo, Llian Mabardi, Ana P Castaño, Yu-Qing Xie, Na Li, Sagar B Kudchodkar, Hing C. Wong, Emily K Jeng, Marcela V Maus and Darrell J Irvine. Enhancing T-cell therapy through TCR signaling-responsive nanoparticle drug delivery, Nature Biotechnology, DOI: 10.1038/nbt.4181