Scientists reveal why some people with the flu may be more contagious
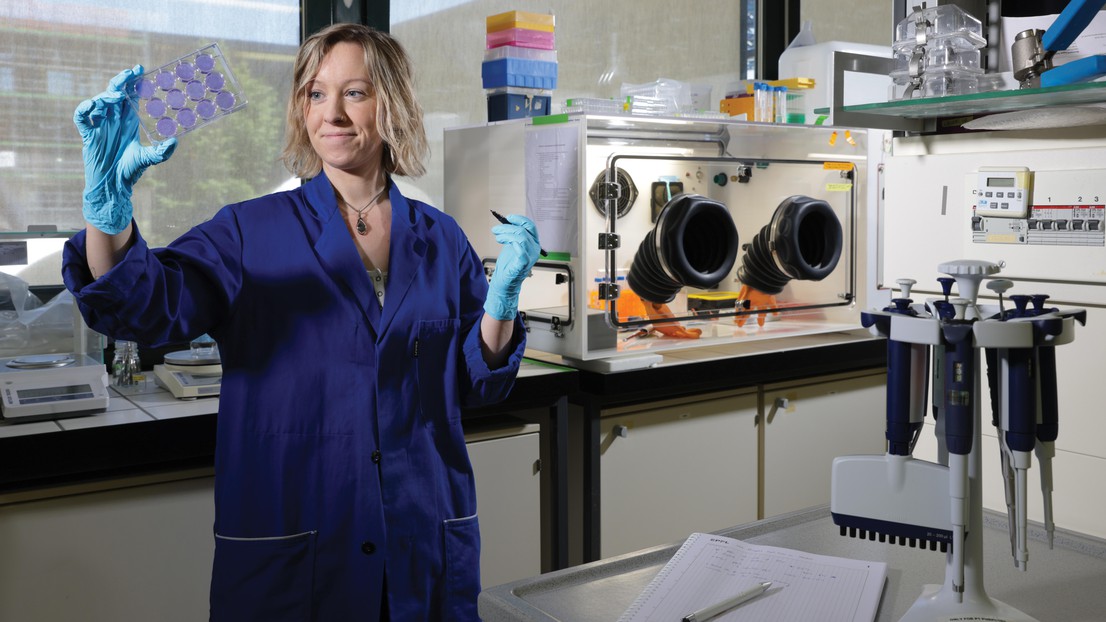
EPFL researcher Shannon David in the Laboratory of Experimental Virology (LEV) at EPFL. 2024 EPFL/Alain Herzog - CC-BY-SA 4.0
EPFL scientists have discovered that in indoor spaces, droplets containing the flu virus will remain infectious for longer when they also contain certain types of bacteria found in our respiratory tract. This finding provides important insight into how respiratory infections are transmitted and can enhance estimates of exposure risk.
An EPFL study has shed new light on the complex relationship between viruses and bacteria found in the human body. Even those of us in good health carry many different types of bacteria on our skin and in our gut, nose and mouth. When we catch respiratory diseases like the flu, the viruses live alongside the bacteria in our respiratory tract. But what happens to these viruses when we sneeze, cough, or talk? A new study by scientists at the Laboratory of Experimental Virology (LEV), along with colleagues at EPFL’s School of Architecture, Civil and Environmental Engineering (ENAC), ETH Zurich, and the University of Zurich, looks at the behavior of the flu virus outside the human body, and specifically how this behavior is influenced by respiratory bacteria. The team’s findings were published recently in Journal of Virology.
It’s already been widely documented that some types of bacteria inside the human gut enable viruses to stabilize and live longer. But Shannon David, an LEV researcher, wondered if bacteria from the respiratory tract play the same protective role in droplets expelled from the human body. To find out, she and her colleagues carried out two types of laboratory experiments. In the first, they created droplets similar to those produced when we sneeze and placed them on a flat surface exposed to indoor air. Some droplets contained only the flu virus, while others also had bacteria commonly found in the respiratory tract. The scientists allowed the droplets to dry and then measured the infectious viral load over time. They found that after 30 minutes in droplets with no bacteria, the virus had died off almost completely (99.9%). In droplets containing both the virus and bacteria, the infectious viral load was 100 times greater at this same time-point, and the virus could survive for many hours.
In the second type of experiment, the scientists measured the infectious viral load of droplets in the form of airborne particles. Here, they found that particles containing only the virus were no longer infectious after 15 minutes. But in particles also containing bacteria, the virus was still present after one hour. The bacteria species with the largest stabilization effect were Staphylococcus aureus and Streptococcus pneumoniae, which both commonly colonize the respiratory tract.

Flatter droplets
Next, the scientists wanted to understand how respiratory bacteria are able to protect the flu virus outside the human body. They observed the droplet samples under a microscope. “Droplets containing bacteria tend to be flatter,” says David. “That speeds the evaporation process and leads to faster crystallization of salt in the droplet, enabling viruses to live longer. This can be an important factor in dry environments such as indoor spaces in the winter when the heating is turned on.”
Until now, little was known about the role that respiratory bacteria play outside the human body. These findings provide an important piece to the puzzle of how respiratory diseases are transmitted. And they help explain why viruses spread so easily from person to person.
“Until now, little was known about the role that respiratory bacteria play outside the human body,” says David. “These findings provide an important piece to the puzzle of how respiratory diseases are transmitted. And they help explain why viruses spread so easily from person to person.” The data her team collected will make a useful contribution to research in a number of fields – including public health.
“The models currently used to predict the spread of a virus in an enclosed space don’t account for the bacteria’s protective function,” says David. “That means they’re probably underestimating the risk of infection.” This study could enable researchers to more easily identify individuals who are likely to produce a higher infectious viral load because they carry more protective bacteria in their respiratory tract.