New drug types can help counter antibiotic resistance
EPFL /iStock
EPFL scientists are developing a new approach that can help stem the tide of antibiotic resistance.
“Antibiotic-resistant infections are responsible for over one million deaths every year, including 250,000 children under the age of five,” says Prof. Alexandre Persat, the head of EPFL’s Microbial Mechanics Lab. “For now, physicians have very few other options available. The situation is already catastrophic, and if we don’t come up with an effective response quickly, it will get much worse.”
A highly problematic category of bacteria
Multidrug-resistant bacteria are often the cause of deaths particularly from nosocomial infections, those infections acquired in a hospital or other healthcare facility. “The World Health Organization has called for the development of new types of treatments, and has listed Pseudomonas aeruginosa specifically as a critical pathogen,” says Persat.
P. aeruginosa is precisely the target of Persat’s research. This bacterium can lead to severe infections among immunosuppressed patients and patients suffering from cystic fibrosis (with a 70% incidence rate). What’s more, it’s responsible for 15% of nosocomial infections. “In some cases, the antibiotics of last resort used to treat P. aeruginosa infections – namely, colistin– have already become ineffective,” says Persat. “That means these patients have very little hope of recovery.”
A novel approach based on mechanics
Antibiotic resistance is a global public-health problem. It’s being driven by several factors, including the excessive use of antibiotics in agriculture. “Basic research will play a fundamental role in finding a solution to this problem, because it’s the only way scientists will be able to pinpoint the Achilles heel of certain types of bacteria,” says Persat. “Then we can develop targeted treatments.” His research group is focused specifically on an overlooked property of bacteria: their sense of touch. They have found that bacteria become more virulent when they are attached to a surface.
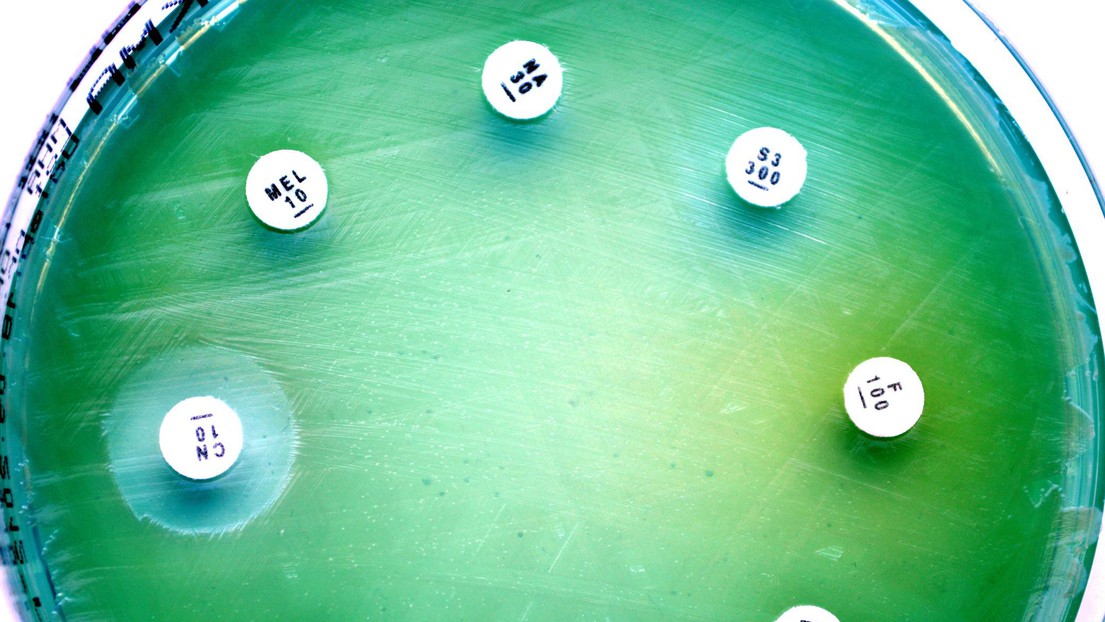
In a study appearing recently in The EMBO Journal, Persat’s research group identified the exact molecular mechanisms that enable P. aeruginosa to feel a surface. “The bacteria are stimulated by contact with a surface, and this seems to be an important factor in the progression of an infection and in the bacteria’s sensitivity to antibiotics,” says Persat. “For instance, in another study we showed that when P. aeruginosa encounters a soft surface, like inside our lungs, it forms a biofilm, which provides the ideal conditions for developing antibiotic resistance. Our discovery will help us and other scientists design new strategies for treating P. aeruginosa infections.”
Deactivating bacteria to prevent infection
New classes of antibiotics are clearly needed to combat multidrug-resistant pathogens. But this approach has its limitations, because sooner or later, bacteria will evolve to become resistant against them too, and continue to propagate and infect people. Another approach, which is also being investigated by Persat, is to “deactivate” bacteria – rather than destroy them – using what are called anti-virulence drugs, or drugs that render bacteria incapable of causing an infection without provoking their own death.
Fondation Jacqueline Beytout
ENABLE and Catalyze for life
Swiss National Science Foundation