Halting the spread of cholera through a neighborhood response

© Delpixart iStock
Using data gathered during a cholera outbreak in Chad, EPFL researchers have found that a response strategy that targets the neighborhood close to reported cases can more effectively contain the outbreak than a large-scale campaign that targets a wider district or an entire city.
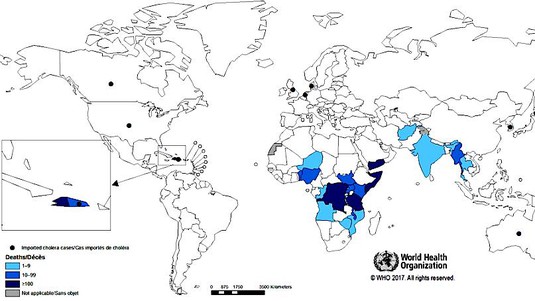
The World Health Organization aims to eradicate cholera by 2030. Through its roadmap, it intends to reduce cholera deaths by 90% and prevent the spread of the disease in 20 cholera-affected countries. Using a mathematical model to process data collected during a cholera outbreak in N’Djamena, Chad, in 2011, EPFL researchers found that a small-scale response that targets the area around households with reported cholera cases could prevent the disease from spreading. Such an approach would require fewer resources and could be implemented more quickly. This type of response would be particularly effective during the early stages of an epidemic, when the number of cases is still low, or to stamp out remaining pockets of the disease after a large-scale response. The researchers’ findings have been published in PLOS Medicine.
EPFL’s Laboratory of Ecohydrology (ECHO) has long been studying the spread of waterborne diseases. It has been focusing on cholera since 2010, when an epidemic in Haiti caused 10,000 deaths. The researchers started out by developing a mathematical model to study the spatial spread of the disease. “The fact that people move about, meet each other and change location was factored into our calculations,” explains Flavio Finger, who has been studying this issue for a number of years at the ECHO lab. These first models were used to gain insight into other epidemics around the globe. Then, to fine-tune their results and ensure they fully reflected the fact that people do not stay in one place, the researchers drew on the mobile phone data of 150,000 users in Senegal during an epidemic there in 2005. This enabled them to map out how the disease had spread.
Putting in place a large-scale response takes time, which gives the outbreak the chance to develop. Nowadays, in addition to understanding how a disease spreads, it’s important to know which response strategies work best and what resources they require. “Our hypothesis was that if those closest to a reported cholera case were treated first, the disease could quickly be prevented from spreading – and this could be done with fewer resources.”

To test his hypothesis, Finger worked closely with Andrew Azman from Johns Hopkins University and other researchers to develop a microsimulation model of the cholera outbreak that swept through Chad, infecting 4,352 people in 232 days. The model incorporated data on both the epidemic curve and the spatio-temporal distribution of outbreaks. The findings of this back simulation confirmed Finger’s hypothesis and demonstrated the effectiveness of a response that focuses on an area of about 100 meters around reported cases. The possible responses involved a combination of treating drinking water, improving sanitation and hygiene, administering oral cholera vaccines and distributing prophylactic antibiotics. By simply distributing the cholera vaccine within a radius of 100 meters of reported cases, for example, the simulated outbreaks were shortened by 68% and the number of cases reduced by 81% compared with the uncontrolled epidemics.
Flavio Finger1¤*, Enrico Bertuzzo1,2, Francisco J. Luquero3,4, Nathan Naibei5, Brahima Toure4, Maya Allan4, Klaudia Porten4, Justin Lessler6, Andrea Rinaldo1,7, Andrew S. Azman6*
http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002509
Press Kit
https://go.epfl.ch/CholeraInterventions
Contacts
Sandy Evangelista Press service EPFL
[email protected]
+41 79 502 81 06
Andrea Rinaldo Director of the Laboratory of Ecohydrology
[email protected]
+41 21 693 80 34
Flavio Finger
[email protected]

https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002509