EPFL and Harvard Join Forces to Diagnose Hearing Loss
© 2012 EPFL
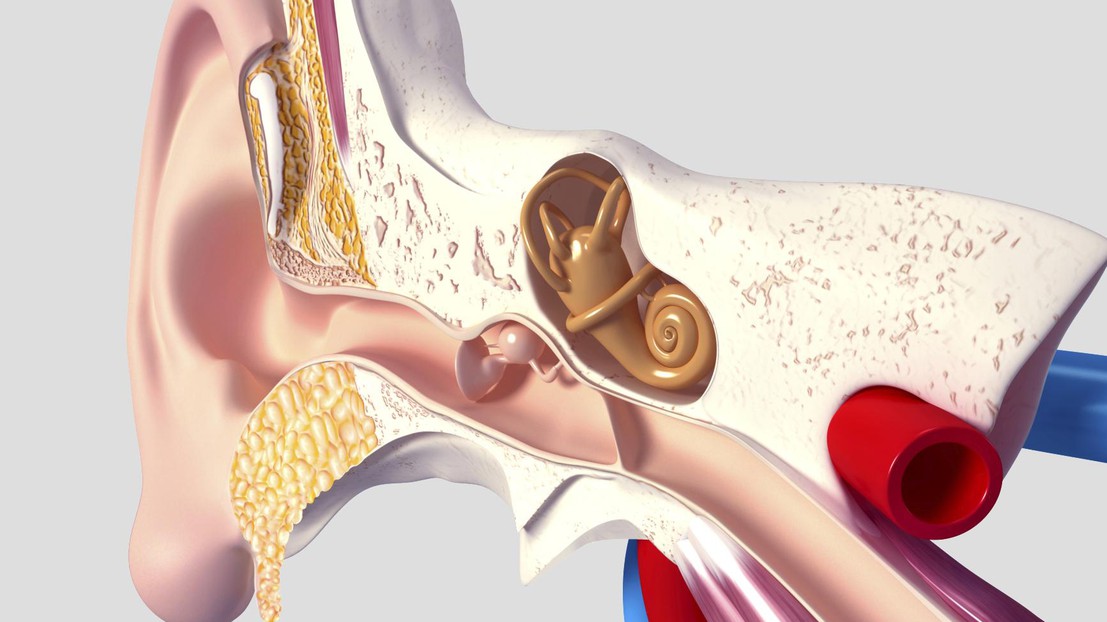
Researchers at EPFL and Harvard Medical School have joined forces to develop an imaging technique that can provide in situ observations of the internal ear, an area which has until now been inaccessible. This groundbreaking work may finally make it possible to understand the mechanisms underlying hearing loss.
What actually causes hearing loss in humans? And what are the best therapeutic approaches to this problem? Modern medicine hasn't yet been able to provide doctors with the right answers in many cases, because there has been no way to observe the tissue of the inner ear, without destroying it. This situation was the starting point for a team of scientists from EPFL's School of Engineering (STI) and Harvard Medical School. They have been working together to develop a non-invasive laser technique that provides extremely high definition imaging of cells inside the cochlea, a narrow, fragile organ within the ear. Early results from testing on mice have been very promising. They have been presented recently at the Bertarelli Symposium at EPFL, and will also appear in the online and print version of the Journal Of Biomedical Optics.
Observing without destroying
The team's new optical method is groundbreaking in that it provides extremely clear images of inner ear tissue without any need for fluorescent labeling of the cells with antibiotics, proteins and other fluorescent markers that are usually used to "color" the targeted cells. This represents an enormous advantage compared with the traditional microscopic methods considered in recent years, which require fluorochrome markers and are therefore impossible to use in clinical practice. "The markers irreversibly damage the tissue, which skews the analyses,"comments Xin Yang, co-author of the article and a doctoral assistant in Demetri Psaltis's Optics Laboratory (LO) at EPFL. As for Magnetic Resonance Imaging (MRI), its resolution is inadequate for observing deep tissue cells. "MRIs can't get beyond 40 microns (a micron equals one thousandth of a millimeter) and the cells we're looking at are on the order of two microns," says Yang.
Autofluorescent cells
To overcome the various obstacles in their path, the team takes advantage of the autofluorescence of the cells in the cochlea. Autofluorescence refers to a phenomenon where certain cells tend to remit light after absorbing it. This phenomenon makes it possible to do without external fluorescent markers. The principle is simple: a laser is aimed at a specific target, causing the absorption of the photons by the cells' molecules. This excites the electrons, and a photon is emitted in return. These photons are then analyzed, providing a high quality image. "To achieve better penetration into the tissue and a higher resolution 3D image, we use a method called two-photon microscopy," says Yang. "This technique consists in directing ultrashort femtosecond laser pulses towards the cells. Thanks to the long wavelength of this kind of laser, the light gets less scattered in the tissue than in the one-photon technique and can go deeper into it. What makes it so efficient is that the molecule can absorb two photons simultaneously, and emit only one, with equivalent wavelength as if only one had been absorbed. In this way, we get very high definition images."
A new method for endoscopic exams?
To test their approach experimentally the team used two populations of mice. One of the two groups was exposed to sounds that caused permanent damage to their inner ears, while the second group experienced a normal environment. The mice in both groups were then put down and their cochleas were removed. The scientists used their laser method and compared the results they obtained from each group. "Among subjects exposed to the sounds, we observed irregularities in the way the cells were aligned and even some missing cells," says Yang. Among the healthy population, the cells were extremely regular.
The next step for the team will be to adapt the new method for use on living subjects. They are working on an endoscopic technique that would guide the laser into the inner ear, thereby eliminating the need to extract the cochlea. "We're planning to use optical fibers measuring about 50 microns to guide the laser," says Yang.
A 3,6 millions francs collaboration
The Journal of Biomedical Optics article is the first publication to come out of the collaboration initiated in April 2011 between the EPFL and Harvard Medical School. The project's objective is to improve quality of life for people with neurological problems by bringing neurosciences and engineering closer together. It is funded by the Bertarelli Foundation, which has made available CHF 3.6 million. The collaboration comprises six cutting edge projects, ranging from diagnosing hearing loss to spinal cord stimulation for paraplegics. A Bertarelli Symposium on the various projects takes place each year, alternating between Harvard and the EPFL. This year's Symposium has taken place October 11th and 12th at the EPFL.
Details: Bertarelli Program in Translational Neuroscience and Neuroengineering
---
Title of publication: Two photon microscopy of the mouse cochlea in situ for cellular diagnosis
Researchers involved:
EPFL: Demetri Psaltis, director of Optics Laboratory
Harvard/Mass. Eye & Ear Infirmary: Konstantina Stankovic