A Promising Future for Soft Bioelectronic Interfaces
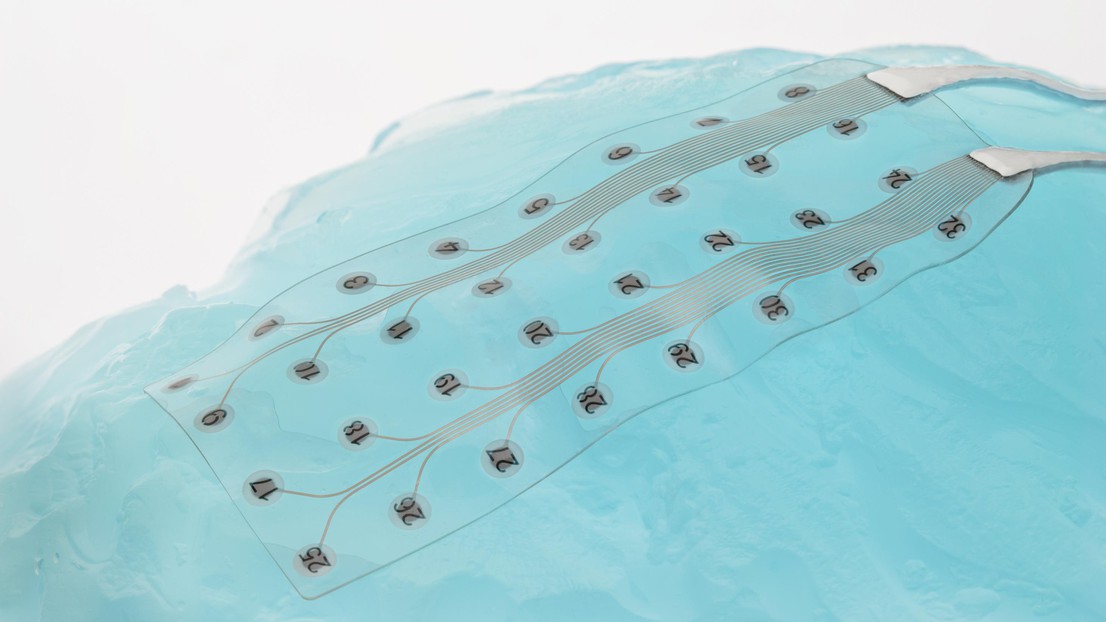
© 2021 EPFL
Results demonstrate magnetic resonance imaging (MRI) compatibility, good surgical handling and reliable recording in bioelectronic interfaces that conform to the nervous system
A new study published in Advanced Science by researchers from the Laboratory of Soft BioeElectronics Interfaces (LSBI) at the Center for Neuroprosthetics, Institute of Bioengineering and Institute of Microengineering (School of Engineering), led by Prof. Stéphanie P. Lacour, has demonstrated MRI compatibility in their soft electrode arrays – a crucial step in translation to the clinic. The work, which received support from the Wyss Center for Bio and Neuroengineering in Geneva and from the Bertarelli Foundation, also confirms the reliable recording of these soft electrode arrays in animal models and surgical handling in human anatomy.
Neural implants can be used to diagnose and treat neurological disorders like epilepsy by electrically recording from the surface of the brain during surgery. However, the long-term success of current neural interfaces is limited by the mechanical mismatch between stiff electronics and soft living tissues.
At the LSBI, advances in stretchable electronics have enabled the development of electrode grids optimized for human anatomy using thin silicone films. This material has the same mechanical properties as the dura mater, the membrane covering the brain, and thus can conform to its complex shape.

Working with clinicians at local hospitals, Prof. Jocelyne Bloch at CHUV (Lausanne) and Prof. Karl Schaller at HUG (Geneva), the LSBI team trialled the surgical handling of the soft electrode grids in human anatomy post-mortem. The clinicians found that the grids can be handled as well as existing devices while conforming better to the shape of the brain tissue. The soft materials enabled the compliant grids to follow the contours of brain folds such as the lateral sulcus, which contains brain regions responsible for speech and hearing, and is not accessible with current devices.
Once implanted, the soft electrode arrays were successfully imaged using a powerful clinical 3T MRI scanner and precisely showed the electrode location in the sulcus as well as the brain tissue around it.
“By using thin silicone membranes, we created devices that the neurosurgeon could handle easily but still enabled a good contact with the brain, a perfect compromise.” says Florian Fallegger, the article’s lead author a post-doc at the LSBI and CTO of Neurosoft Bioelectronics.

The devices are created using microfabrication processes borrowed from the integrated electronics industry which enables the electrode shape to be tailored to the needs of the user. As part of the study, the ability of different electrode designs to record brain activity was trialled in minipig models in collaboration with scientists at Clinatec (Grenoble).
“This work underlines our efforts to push new and innovative technology to the clinic” says Prof. Stéphanie Lacour, Bertarelli Foundation Chair in Neuroprosthetic Technology at EPFL, “by involving engineers, neuroscientists and clinicians in the research process from the very start, we improve our chances of successful translation”.
The technology is now being translated to the clinic by a spin-off from the LSBI, Neurosoft Bioelectronics, enabled by the results of the collaborative work. The Wyss Center is working with the Neurosoft Bioelectronics team to help validate their electrodes for use in humans and drive eventual commercialization.
Bertarelli Foundation
Wyss Center for bio‐ and Neuroengineering