A link between sensory neurons activation and the immune system
© 2020 EPFL
Scientists at EPFL, ETH Zurich and Harvard Medical School/Boston Children’s Hospital have developed an implantable technology that enabled the discovery of an interaction between sensory neurons and immune cells.
Pain is a protective mechanism, alerting us to danger by generating an unpleasant sensation. The warning message is carried to the spinal cord by specialized sensory neurons, which are intertwined with other sensory and motor neurons in peripheral nerves. If injury cannot be avoided, inflammation arises and is associated with redness, swelling and pain. “For a long time, pain and inflammation were thought to be distinct processes, generated independently. Whether the sensory fibers that trigger pain can induce inflammation has never been shown before” indicates Frédéric Michoud, a post-doctoral fellow at EPFL. Such a neuroimmune interaction if present would have implications for future treatments of inflammation. The study published in Nature Biotechnology using the new neurotechnology shows that this is the case.
Selective stimulation of sensory neurons with light
Optogenetics is a technique allowing for modulation of genetically-selected neurons by shining light into neural tissues. Although optogenetics has revolutionized neuroscience focusing on the brain, its application to neurons in peripheral nerves has been difficult. "The challenge has been to develop a technological approach that allows optical stimulation/illumination to occur repeatedly over many days without damaging the nerve and impacting the behavior of the animal” says Professor Clifford Woolf of Harvard Medical School/Boston Children’s Hospital.
An optoelectronic implant around the sciatic nerve
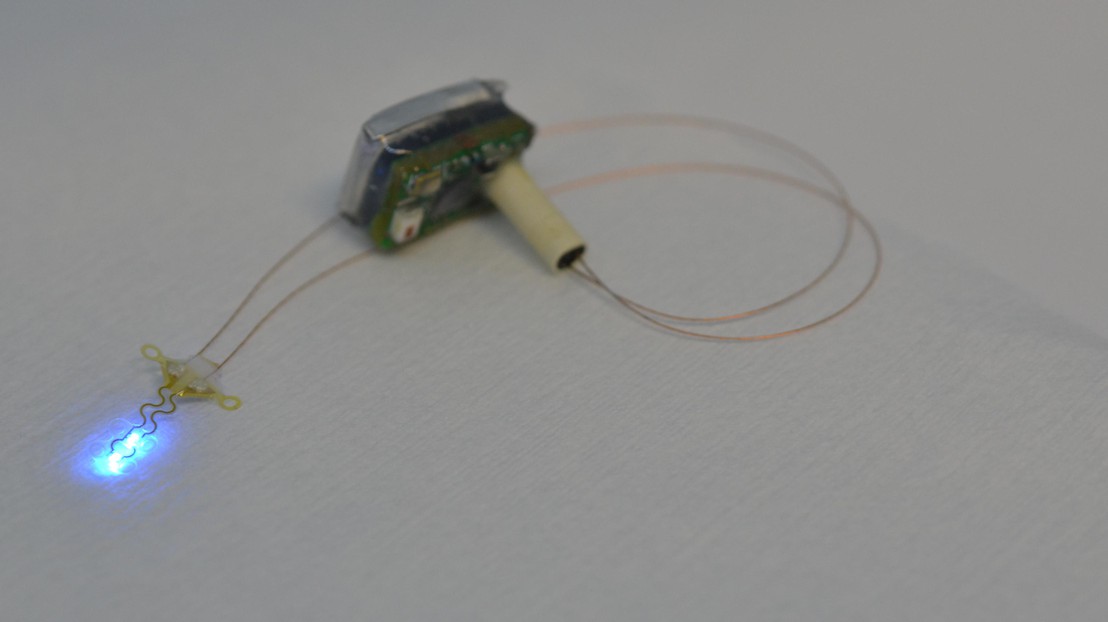
Researchers at the Bertarelli Foundation Chair in Neuroprosthetic Technology developed a soft implant that wraps around the sciatic nerve and delivers blue flashes of light on demand. “In the compliant implant, we have integrated several light-emitting diodes. The advantage is that we can control the illumination electrically," explains Stéphanie Lacour, Professor in the Faculty of Engineering Sciences and Techniques. This implant is connected by a subcutaneous cable to an electronic system secured on the top of the head of the mice. “Our colleagues at ETH Zurich have developed a miniaturized chip for controlling the implanted diodes, that is energy efficient and integrated into a wireless communication interface. Thanks to this system, we can control exactly when and how the implant is activated, regardless of what the animal is doing”, explains the scientist. Control tests confirmed that the optoelectronic implant did not interfere with the animal's behavior in any way and did not induce side effects.
Activation of pain-triggering sensory fibers initiates and amplifies inflammation
To the team’s surprise, the repeated optical stimulation of specific sensory neurons in the nerve produced mild redness in the animal’s hindpaw, a clear sign of inflammation, further confirmed by quantified analyses of immune cells present in skin samples. “Our study has provided an answer to the long-held question of whether those neurons that produce pain also produce immune-mediated inflammation – the answer clearly is, yes!” concludes Clifford Woolf.
This miniaturized implantable neurotechnology paves the way for many other studies that will allow investigators to decipher and unravel peripheral and central neural circuits, and possibly define future approaches to treat syndromes such as chronic pain or persistent inflammation.
The Bertarelli Foundation
SNSF
NIH
Wellcome Trust and the Royal Society (the European Union’s Horizon 2020 Research and Innovation Programme under the Marie Skłodowska-Curie grant agreement