When false alarms pollute intensive care
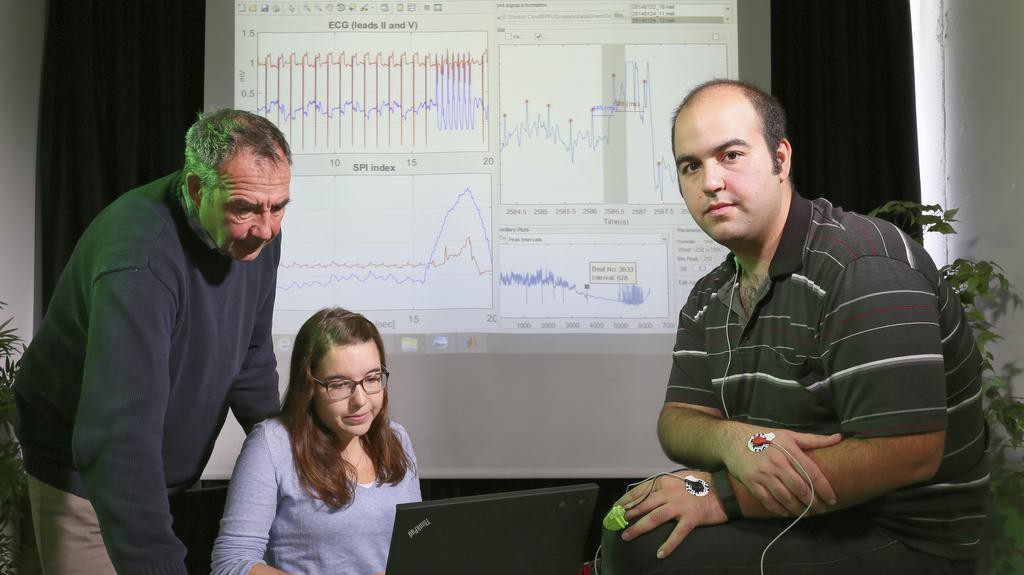
© 2015 Alain Herzog EPFL
Two EPFL doctoral students created algorithms capable of eliminating false alarms that pollute intensive care units. To do this, they came up with the idea of pairing electrocardiogram data with optical waveform data. Their work has won top honors at the Computing in Cardiology conference at MIT.
Intensive care units are known for their incessant symphony of alerts. 90% of them are false alarms, and they are so common that medical staff no longer pay them much heed. These false alarms are the result of several factors, such as when electrodes placed on the patient move, causing artifacts that trigger an alert. The alerts stream forth, filling the air day and night. They have a negative impact on both patients and medical staff: they disrupt the patients’ sleep, but, more importantly, they cause alarm fatigue among staff.
This very topic – reducing false arrhythmia alarms in the ICU – was the focus of the 2015 Computing in Cardiology conference. This annual conference, organized in conjunction with MIT, features a competition involving the application of computers in the area of cardiology in order to improve patient care. Sibylle Fallet and Sasan Yazdani, PhD students at EPFL’s Applied Signal Processing Group (ASPG), took up this year’s challenge. The approach they developed, which cut the number of false alarms in half, earned them first place in the competition.
Bradycardia, tachycardia, asystole, arrhythmia, fibrillation – the two EPFL doctoral students had to quickly master the medical jargon since their research focused on signal analysis in cardiology. “This challenge was right in line with their respective projects,” said Jean-Marc Vesin, Senior Scientist at the ASPG. “Sybille is working on an algorithm for instantaneous estimation that will, among other things, help in monitoring the vital functions of premature babies, and Sasan developed an algorithm capable of reliably detecting R wave peaks in ECGs, something that will improve sensors embedded in smart clothes, for example.”
Like all the other competitors, the EPFL students were given the electrocardiograms of 1,250 patients. “We were provided with different signals. Even if they weren’t always high quality, most of the time we had the ECG and visual data from the PPG, which is read by placing a sensor on the patient's finger,” said Sibylle. The PPG – short for photoplethysmograph – uses light absorption technology to detect waves produced by the body’s pulse.
The real hurdle in this type of exercise is to precisely measure the heart rate. Because the quality of the signals can vary, catching each beat is no mean feat. The two algorithms developed by Sibylle and Sasan pick up where the other leaves off. If electrical activity does not show up clearly on the electrocardiogram, the photoplethysmographic waveform can provide the missing data.
“Thanks to this dual monitoring, we eliminated 87% of the false alarms while effectively detecting real alerts,” said Sibylle.
“When we were working on this we kept in mind that it could be attached to real intensive-care monitors, so most of our algorithms work in real time and don’t require much memory to do the calculations,” said Sasan.
---
The researchers will publish an article in an upcoming issue of Physiological Measurement. Sibylle Fallet and Sasan Yazdani’s work was carried out under the Nano-Tera initiative, which is funded by the Swiss government.


