Study finds indigenous cases of leprosy in the Southern United States

© 2011 Heidi and Hans-Jürgen Koch
Study confirms human contamination through contact with armadillos
Using advanced DNA analysis and extensive field work, an international research team has confirmed the link between leprosy infection in Americans and the presence of armadillos. In a joint collaboration between the Global Health Institute at EPFL in Switzerland and the National Hansen’s Disease Program, clear evidence was found that a never-before-seen strain of Mycobacterium leprae has emerged in the Southern United States and that it is transmitted through contact with armadillos carrying the disease. The results will be published on April 28th in the New England Journal of Medicine.
There are only around 150 cases of leprosy in the United States each year. Most of these individuals have lived or worked abroad in areas in which leprosy is endemic, making it likely that they have acquired the disease while outside the US. But, to the alarm of health authorities, a third of all patients infected appear to have contracted the disease locally. The hypothesis that the disease is transmitted though contact with armadillos—aside from humans, the only other known carriers of the leprosy-causing bacteria—was confirmed by fine-grained DNA analysis of both armadillo and human samples done at EPFL.
Leprosy bacilli found in armadillos
It has been known since the 1970s that armadillos are potential carriers of the disease, most likely introduced by European immigrants 500 years ago. But the current study shows inter-species contamination and the presence of a unique strain. “There is a very strong association between the geographic location of the presence of this particular strain of M. leprae and the presence of armadillos in the Southern US,” explains Stewart Cole, head of the Global Health Institute in Lausanne and world-leader in the field of genomics of leprosy bacilli. “Our research provides clear DNA evidence that the unique strain found in armadillos is the same as the one in certain humans.”
The study included 33 wild armadillos known to have the disease and 50 leprosy patients. The new strain of the bacterium, named 3I-2v1, was found in 28 armadillos and in 22 patients who reported no foreign residence. The researchers used genome sequencing to identify the new strain and cross check it with other known strains from Europe and Asia, and used genotyping to identify and classify the population infected. It became clear that leprosy patients who never travelled outside the US but lived in areas where infected armadillos are prevalent (see map) were infected with the same strain as the armadillos. These findings prompted the researchers to state in the article that “Frequent direct contact with armadillos and cooking and consumption of armadillo meat should be discouraged.” The study also suggests that armadillo range expansion should be monitored.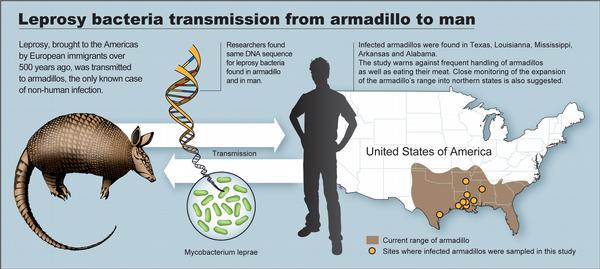
It is not known exactly why armadillos contract and carry leprosy. While their low body temperature (89° F / 32° C) makes them perfect incubators for the bacteria, which grow in temperatures between 86° F and 89° F (30° C to 32° C), there are almost certainly other factors such as immune deficiency that also play a role. Similarly, the bacteria attack the extremities of humans because our core body temperature is too high for a generalized infection, and over 90% of humans who come into direct contact with the disease spontaneously fight it off. “ The best way to combat further infection is though education and prudence,” says Cole.
The stigma of leprosy
José Ramirez, a former migrant worker from Houston who contracted the disease after hunting and eating armadillo meat.. He hopes that the study brings to light the stigma attached to leprosy. “We need to take this opportunity to give leprosy patients a voice and to learn to not use the word ‘leper’ that has negative connotations around the world, a stigma that should be replaced with an understanding of the disease and its causes.” Ramirez, who struggled over five years with the disease before it was properly diagnosed, is now disease-free after receiving antibiotic treatment. Proving what few know to be true -- that leprosy is a bacterial infection that can be cured.