Rehabilitation after a stroke: an interview with Friedhelm C. Hummel
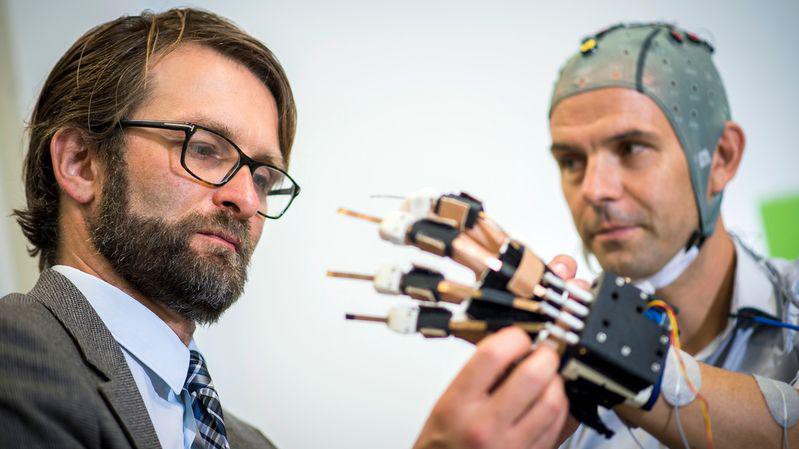
Friedhelm Hummel with a stroke patient © RTS/Olivier Maire - Keystone
Friedhelm C. Hummel recently joined EPFL’s School of Life Sciences, Brain Mind Institute (BMI) and Centre of Neuroprosthetics (CNP) as a Full Professor (Defitech Chair of Clinical Neuroengineering).
Professor Hummel is a fully trained neurologist and, besides being a researcher, has also worked as a clinician. In the last few years he worked at the University Medical Center Hamburg-Eppendorf in Germany as Vice Director of its Department of Neurology, and headed its Brain Imaging and NeuroStimulation Laboratory.
He recently joined EPFL’s School of Life Sciences (Brain Mind Institute) as Full Professor, and he now heads a lab that focuses on research and treatment of stroke.
Tell us a bit about your background. What questions led you to your field of research?
I dedicated the last 10-15 years of my research towards translational research in stroke. It is a very frequent disease and the main cause of long-term disability. Stroke has an unsatisfactory functional recovery and significant consequences for the patients, their social environment and the health system overall.
My research has two main goals: First, to better understand the underlying mechanisms of neuronal reorganization and functional recovery after a stroke on the level of a systems neuroscience network. Second, to develop novel treatment strategies, especially interventional strategies based on non-invasive brain stimulation, that can further enhance residual motor and cognitive functions and thus help with functional recovery.
Besides this, focal lesions in the brain [the injured areas in the brain after a stroke], provide a good scientific model to better understand the capacity and mechanisms of the brain for neuroplasticity and reorganization, and to do so from the point of view of a brain network.
In later years, the topic of healthy aging and processes underlying healthy aging became my second main research topic. The neuroscience of aging systems is of high interest and relevance due to our aging society, and the fact that in a few years aged subjects will be the main labor force.
In our fast-changing communication and computer-driven society, the ability to acquire new skills is outstandingly important for staying integrated and participating in normal professional or private life -- even at an advanced age. Thus, in current research, I address questions of neuroplasticity, structural and functional change, and skill acquisition during healthy aging, and look at how age-related impairment can be influenced by means of non-invasive brain-stimulation.
What are you currently researching?
Thus far, the effects of neuro-rehabilitative treatment and other novel strategies, leave much to be desired. It is becoming increasingly clear that the concept of "one treatment suits all" does not lead to satisfying improvements of behavioral deficits after stroke.
So we are currently exploring ways to improve the effects of interventional strategies that support residual function and functional regeneration after stroke. To this end, we are using multimodal imaging to develop factors that can predict individual residual function, the course and key players (e.g. in the motor network) of functional recovery, and the magnitude of response, for example, to brain stimulation.
Why is it important?
These projects will be crucial in forming the basis for the development of individualized, patient-tailored treatment strategies -- especially those that rely on non-invasive brain stimulation -- to maximize the effects of neuro-rehabilitation for patients. And we are also testing applications of these interventions that can allow patients to do high-intensity neuro-rehabilitative training at home. The brain stimulation in this set-up is controlled remotely by us.
What experimental methods do you use?
Our aim is to understand the underlying processes of healthy aging and functional regeneration after stroke. To do this, we use a multimodal, systems-neuroscientific approach, which includes fMRI, structural MRI, electroencephalography, single- and paired-pulse transcranical magnetic stimulation.
We also use neuromodulation by transcranial electric or transcranial magnetic stimulation, which focuses on changes in cortical plasticity, intracortical and cortico-cortical interactions, structural and functional connectivity, and behavior.
How do they help you pursue your research goals?
This multimodal-approach, which exploits the complementary strengths of different methods, allows us to best address our research questions in both healthy subjects and patients. Prospectively, this approach could also allow us to determine a method or the combination of methods that are most predictive for the course recovery of the patients.
Our lab includes an interdisciplinary team of MDs, biologists, neuroscientists, physiotherapists, and engineers. This enables us to employ these methods with excellence, but to also apply them in a clinical context, which is important for translational research from bench to bedside.
What is your future research vision?
The degree of residual deficits, especially in hand function, is one of the key obstacles that determine the patient's ability to reintegrate into normal social and professional life, and to enjoy independence and quality of life. Though there are recent developments that improve the effects of the neurorehabilitative treatments, their impact is not satisfactory, leaving too many patients significantly impaired.
One of the reasons that novel, interventional treatment strategies can't offer larger benefits might be that they are used as "one treatment suits all" applications. Such an approach does not take into account that, even if the initial impairment of stroke patients is similar, the course of recovery, the underlying mechanisms of recovery, and the degree of residual impairment might differ significantly depending on factors such as the size and location of the focal lesion as well as other structural and functional aspects.
What would you like to accomplish, in and out of the lab?
There is a very exciting environment here at EPFL, and especially at the BMI and the CNP. Combining all their different kinds of expertise we can optimize the use of multimodal systems neuroscience and complex data analysis. Meanwhile, we have the unique option of having a basic systems neuroscience laboratory at Campus Biotech (Geneva) as well as a translational laboratory at the Campus Sion (Clinique Romande de Réadaptation, EPFL Valais Wallis) to test our translational research ideas in a clinical environment.
So I hope that with all these resources we will facilitate the evolution from "imprecision medicine" and "one treatment suits all" towards patient-tailored, “precision-medicine” approaches that adjust and adapt to the patient's individual requirements to maximize their treatment success.
These goals can only be achieved as an interdisciplinary team with different expertise from engineering, electrophysiology and imaging to clinical evaluation and big data analysis. I have built and always am building up my team towards this expertise and goals.
Furthermore, the rich and exciting research environment at EPFL, with its international research community, provides a fertile ground for collaborations. Speaking with other researchers, I have already experienced the strong commitment and desire for cooperation within the BMI and wider EPFL family.